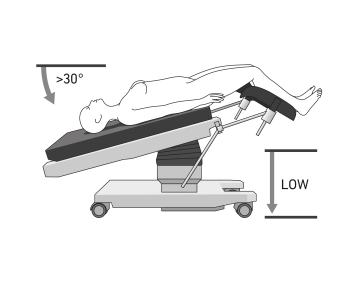
- positioned in lithotomy position
- It is recommended to position both arms alongside the body (caution: use cotton wrapping when positioning with a cloth sling), or to position one arm on the assistant's side
- The legs should be adjustable via the operating table controls
- if necessary, use shoulder supports to prevent the patient from slipping on the operating table
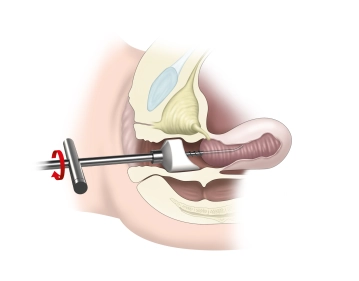
- Insertion of a transurethral bladder catheter
- Attachment of a cervical adapter
-
Positioning
![Positioning]()
-
Anesthesia examination and placement of a cervical adapter
![Anesthesia examination and placement of a cervical adapter]()
Soundsettings Under anesthesia, the mobility and degree of the prolapse are assessed in detail. This includes:
- Prolapse of the anterior compartment (cystocele): Assessment of the bladder base.
- Prolapse of the middle compartment (descent of the cervix)
- Prolapse of the posterior compartment (rectocele): Condition and descent of the rectum.
Placement of the Hohl portio adapter:
A tenaculum is used to securely grasp the portio vaginalis of the cervix. The portio is carefully grasped with the tenaculum. A targeted caudal traction is applied to stretch the uterus and optimize the anatomical conditions. This facilitates the introduction of the further components of the portio adapter. The intracavitary probe is carefully inserted into the cervical canal lumen, taking care not to cause perforation or excessive tension. The threaded piece is securely positioned and fixed into the cervix uteri by rotational movements.
-
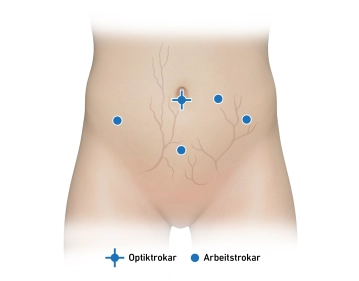
Trocar positioning
![Trocar positioning]()
Soundsettings Incision infraumbilical. Before introducing the Veress needle, the abdominal wall should be lifted to increase the distance from the intra-abdominal organs. Establishment of a pneumoperitoneum by introducing a Veress needle.
TIP: When penetrating the fascia and peritoneum, there are often two distinct resistances. After penetrating the peritoneum, the movement feels free and smooth. Begin the insufflation of CO₂ slowly. An initial pressure below 10 mmHg and a steady pressure increase with constant gas flow indicate correct positioning.
Insertion of the optical trocar. During laparoscopy, inspection of the abdomen is performed, including the upper abdominal area, the diaphragmatic domes, the liver, the gallbladder, the stomach, and the omentum. Additionally, inspection of the intestines and peritoneum is conducted.
Trendelenburg position and placement of 3 additional working trocars under vision.
The selection of the number and position of the laparoscopic incisions is at the discretion of the surgeon and is based on their personal preferences as well as the specific requirements of the operation. Incisions are often chosen in the left and right lower abdomen or in the left and lower and mid-abdomen (left periumbilical).
Procedure for incisions in the lower abdomen: Display the inferior epigastric artery in the lateral umbilical fold. Laterally, the superficial vessels are visualized via diaphanoscopy (superficial circumflex iliac artery, superficial epigastric artery). Two fingerbreadths medial to the anterior superior iliac spine, in the vessel-free area, incision and insertion of a working trocar into the lower abdomen.
Procedure for incisions in the mid-abdomen (mostly left): Display the inferior epigastric artery in the lateral umbilical fold. The superficial vessels are visualized via diaphanoscopy. Incision at the level of the navel and approximately 3 cm lateral to it. It is important to ensure that the incision is not too close to the optical trocar or in line with the working trocar of the lower abdomen, risk of collision.
Procedure for suprapubic incisions: Preoperative placement of a urinary catheter to empty the bladder. 1-2 fingerbreadths above the symphysis, the superficial vessels are visualized via diaphanoscopy. Incision and insertion of the working trocar under vision.
-
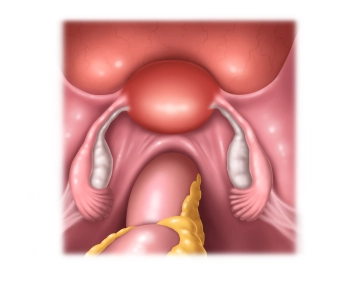
Inspection of the pelvis
![Inspection of the pelvis]()
Soundsettings The inspection of the pelvis is performed systematically:
- Uterus:
- Assessment of size, shape, and mobility.
- Indications of fibroids or suspicion of malignancy?
- Adnexa:
- Ovaries: Assessment of size, shape, color, cysts, or tumors.
- Tubes: Assessment for hydrosalpinx, pyosalpinx, or tumors.
- Peritoneum and Douglas pouch:
- Look for free fluids (blood, pus).
- Assessment for adhesions, endometriosis foci, or tumor implants.
- Bladder and anterior pelvic wall:
- Inspection for abnormalities or injuries.
- Retroperitoneum:
- If possible, assess lymph nodes and vessels.
- Identification of the promontory
- Transperitoneal visualization of the ureter
- Uterus:
-
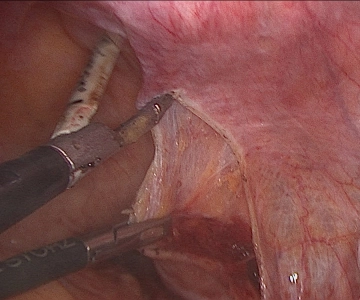
Opening of the retroperitoneum
![Opening of the retroperitoneum]()
Soundsettings The sacrouterine ligaments are identified as they serve as guide structures to the cervix and the promontory. Secure transperitoneal visualization of the right ureter is achieved again.
Opening of the peritoneum at the level of the promontory. The promontory is located as a prominent projection of the sacrum, near the junction with L5. It is gently freed from surrounding tissue and fat using blunt instruments. The median sacral artery and vein, which run directly over the promontory, are visualized and preserved, as is the inferior hypogastric plexus, which runs in the presacral space, identified and not disturbed. The bony surface of the promontory is completely exposed to create a sufficiently large and stable anchoring surface for the later MESH.
Using a portio adapter, the uterus is ventralized. This causes the anatomical structures to tense better and become visualized. After visualizing the promontory, the peritoneum is carefully opened medially along the uterosacral ligaments. Between the posterior vaginal wall and the ventral rectum, the rectovaginal space is freed by blunt dissection. By opening the rectovaginal space, sufficient mobility of the peritoneum is achieved. This is necessary to fully cover the MESH with peritoneum later.
Display of the infundibulopelvic ligament and transperitoneal identification of the ureter. After i
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$52.30/ yearly payment
gynecology
Unlock all courses in this module.
US$104.60 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.