Tenosynovitis of the hand and wrist is a group of entities with a common pathology affecting the extrinsic tendons of the hand and wrist and their corresponding retinacular sheaths. It typically begins as tendon irritation, manifesting as pain and swelling caused by increased production of synovial fluid (tendon sheath hygroma).
The treatment of choice is initially conservative with immobilization of the affected hand section. If tenosynovitis occurs in the context of a specific underlying disease (PCP, psoriasis, LE, etc.), medical treatment with the appropriate antirheumatics should be undertaken.
If conservative therapy fails, removal of the synovia is strongly recommended to stop the inflammatory process. Otherwise, tendon rupture is to be expected.
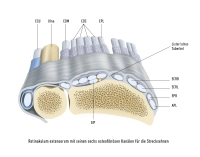
In the present case, it is a special form of tenosynovitis of the 4th dorsal compartment (EDC and EIP) following a malunited radius fracture. The malposition of the bone led to a hypomochlion with narrowing of the tendon canal. Consequently, there was chronic irritation with synovitis and partial tendon rupture. To prevent recurrence, a synovectomy was performed along with a retinaculum plasty (see procedure).
The retinaculum plasty has two goals: It protects the vulnerable tendons from direct contact with the bone, thus preventing renewed mechanical irritation. Additionally, the tendons are re-centered and regain their original straight course.