The indication for open repair of abdominal aortic aneurysm (AAA) basically results from comparing the patient's individual risk of rupture in the spontaneous course of the disease with the risk of open surgery. If the risk of spontaeous rupture over the course exceeds the individual surgical risk, open surgery is usually indicated.
Rupture risk classification
| Factors | Low risk | Moderate risk | High risk |
| Aneurysm diameter | <5 cm | 5–6 cm | >6 cm |
| Growth rate per year | <0,3 cm | 0,3–0,5 cm | >0,5 cm |
| Smoking/COPD | Low | Moderate | High |
| Family history | None | Isolated | Common |
| Arterial hypertension | None | Well controlled | Unstable despite treatment |
| Morphology | Fusiform | Saccular | Evaginations |
| Gender | Male | Female |
Indication for surgery
| Classification | Size | Wall | Presentation | Indication for surgery |
| Asymptomatic infrarenal | >5 cm ♂ >4.5 cm ♀ | Intact | None | Elective |
| Asymptomatic supraaortic | >6 cm | Intact | None | Elective |
| Symptomatic | Independently of other factors | Intact | Spontaneous pain; tenderness in abdomen, back or side | Urgent, within 24 hours |
| Ruptured | Independently of other factors | Contained or free rupture | Diffuse severe spontaneous pain / tenderness of tense abdomen, with/without hemorrhagic shock | Emergency |
| Aortoduodenal fistula | Intermitted vomiting, melena | Emergency | ||
| Aortocaval fistula | Right heart failure, fistula bruit, truncal cyanosis, concurrent contrast enhancement of aorta & inferior vena cava | Emergency |
There are two types of repair in AAA:
- open replacement of the abdominal aorta with a straight (tubular) or bifurcation graft (OAR, open aortic repair)
- endovascular placement of a stent graft (EVAR, endovascular aortic repair)
Laparoscopic aneurysm repair surgery, usually performed in combination with mini-laparotomy, is of lesser importance.
The following recommendations serve as a guide to choosing between OAR and EVAR:
OAR (trans-/retroperitoneal)
- Normal life expectancy
- Low surgical risk (fitness)
- Anatomy unsuitable for EVAR: landing zone; aneurysm neck (angle, length); iliac vessels (stenosis, elongation, kinking); thrombi; calcification
- Marfan and other connective tissue disorders
EVAR (standard /customized graft)
- Prior abdominal surgery
- Limited life expectancy
- High surgical risk
- Anatomy suitable for EVAR (see above)
Since stent graft systems are often of large caliber, EVAR requires adequate iliac artery lumen for access. Iliac arteries with atherosclerotic stenosis, tortuosity, kinking, or aneurysmal dilation are a problem.
In the long run, endovascular aortic grafts are associated with a higher complication rate than open aortic surgery.
The BAR Score Calculator -> www.britishaneurysmrepairscore.com can quickly calculate patient mortality risk for EVAR or OAR, which can be useful when advising patients about the risk of elective EVAR or OAR.
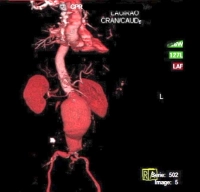
Video example:
Asymptomatic infrarenal AAA greater than 5 cm in diameter do not lend themselves to EVAR due to aneurysmal neck angulation greater than 60°.