According to the TASC criteria, therapeutic treatment options can be derived depending on the local occlusion/stenosis length. The length of the stenosis and its localization regions decide on the therapy: endovascular or open vascular surgery.
TASC criteria of aortoiliac vascular occlusions
Types | Morphology | Therapy principle |
|---|---|---|
A | Focal stenoses of the A. iliaca communis or A. iliaca externa <3 cm, uni- or bilateral | endovascular |
B | Focal stenoses 3–10 cm long and/or unilateral occlusion of the A. iliaca communis | endovascular |
C | Bilateral stenoses of the A. iliaca communis, 5–10 cm or unilateral complete occlusion of the A. iliaca externa or bilateral occlusions of the A. iliaca communis | open reconstruction |
D | Diffuse stenotic changes of the entire iliac axis or unilateral occlusion of the A. iliaca communis and externa or bilateral occlusions of the A. iliaca externa | open reconstruction |
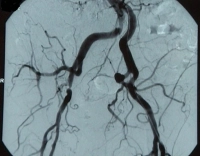
Video example: TASC B, high-grade stenosis of the A. iliaca externa and 50 % stenosis of the A. iliaca communis on the right, clinically PAOD stage IIb according to Fontaine → Indication for endovascular reconstruction
Fontaine stage | Clinical presentation | Rutherford category | Grade | Clinical presentation |
|---|---|---|---|---|
I | asymptomatic | 0 | 0 | asymptomatic |
IIa | Walking distance > 200 m | 1 | I | mild claudication intermittens |
IIb | Walking distance < 200 m | 2 | I | moderate claudication intermittens |
| 3 | I | severe claudication intermittens | |
III | ischemic rest pain | 4 | II | ischemic rest pain |
IV | Ulcer, gangrene | 5 | III | minor tissue loss |
6 | III | major tissue loss |