The diagnosis of acute limb ischemia can often be made "at a glance" after a brief history and examination. Normally, angiography is not performed (exception: concurrent PAOD) and management is planned based on the clinical findings (history, inspection, palpation). After having resolved the absolute ischemia, diagnosis and treatment of the source of the embolism can be approached in orderly fashion.
Emergent diagnostic work-up should address the following questions:
- Severity of ischemia (Pratt's 6 Ps, TASC in PAOD)?
- Localization and extent of the occlusion?
- Acute ischemia resulting from embolization or PAOD?
The typical 6 Ps of Pratt characterize the severe course of acute limb ischemia with grave threat to the limb viability (Source: Pratt GH (1954) Cardiovascular surgery. Kimpton, London):
In PAOD, the classification of acute limb ischemia according to the Transatlantic Inter-Society Consensus (TASC) Working Group seeks to reflect the varying levels of urgency for further diagnostic work-up and management:
Medical history/clinical picture
Rough distinction between acute thrombotic occlusion and embolism:
→ Embolism
- Sudden, occasionally whip-like pain in the limb (cardinal symptom)
- Often severe ischemia
- Cardiovascular history: known atrial fibrillation; heart defect; history of myocardial infarction; aortic aneurysm
→ thrombotic occlusion
- more likely symptoms increasing over several days, typically with incomplete ischemia
- Known PAOD (claudication symptoms?)
- History of bypass surgery, stenting/PTA
- Atherosclerosis risk profile
- Local trauma
- No evidence of source of the embolism
Skin color
- White ischemia: pale distal to the occlusion
- Blue ischemia: less favorable prognosis because thrombus formation due to stasis has already spread to the venous circulation
- Spontaneous Ratschow test may be seminal in incomplete ischemia (total pallor with the limb elevated and no recovery even after returning the limb to the horizontal position).
Capillary refill time
- short plantar pressure with finger on big toe or forefoot → initially pale pressure point usually turns red within < 3 seconds
- The longer the redness takes to appear, the more marked is the perfusion disorder
Effective perfusion pressure
- Elevation of the limb allows the perfusion pressure to be estimated → 10 cm = 7.5 mmHg
Skin temperature
- The affected limb is colder when comparing both extremities
- The occlusion is much more proximal than the drop in temperature
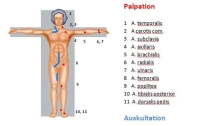
Pulses
- In the simplest case, lack of pulses in the affected limb
- Bilateral lack of pulses: pre-existing bilateral PAOD or asymptomatic embolism
Auscultatory bilateral comparison of the limb arteries
Ankle-Brachial Index (ABI)
- ABI = systolic BP of posterior tibial artery / systolic BP of brachial artery
- the smaller the ABI, the more pronounced the ischemia
- In acute stages, the pressure might not be measurable
Color-flow Doppler ultrasonography
- Carotid artery, abdominal aorta, limb arteries (rule out popliteal aneurysm in lower leg occlusion!)
- Stenoses and occlusions in almost all vascular regions apart from chest
- Allows quantifying the degree of stenosis and assessing plaque morphology
- Sensitivity and specificity around 90%
CT angiography
- Multislice computed tomography (MS-CT) with nonionic contrast agent
- Broad range of indications: traumatic vascular lesion (esp. trunk); vascular dissection/rupture; aneurysm; arterial thrombosis/embolism; portal vein/mesenteric vein thrombosis; pulmonary artery embolism; PAD; vascular tumors
- Benefits: rapid; detects relevant comorbidities; visualizes peripheral arteries; sensitivity and specificity each about 90%
- Drawbacks: Radiation and contrast agent exposure, allergies (about 3%), no functional assessment
- Indication does not depend on the degree of ischemia but on the history and clinical findings in the contralateral leg: angiography is recommended in case of pre-existing PAOD or evidence of popliteal aneurysm. The findings then determine the surgical strategy. The presence of concomitant PAOD or popliteal aneurysm as the origin of acute ischemia necessitates more complex repair (e.g., interposition grafts, bypass procedures). However, in case of complete ischemia do not waste too much time on angiography (suitable logistics).
Laboratory panels
- Blood count
- Electrolytes
- Coagulation
- Kidney function parameters
- Liver function parameters
- Blood lipids
- Blood group
Cardiac check
Chest x-ray
As an emergency measure administer 5000-10000 IU heparin to prevent appositional thrombosis. Protect the foot in a padded bootie to prevent pressure injury (especially during surgery as well!).