Longitudinal incision at the anterior border of the left sternocleidomastoid muscle. Division of the subcutis and platysma, subtle hemostasis.
-
Left cervical access
-
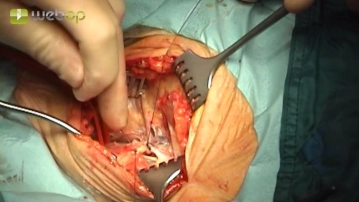
Preparation of the ACC
![Preparation of the ACC]()
Soundsettings Exposure of the anterior side of the common carotid artery (ACC), which is then encircled and looped with a Vessel Loop as a tourniquet.
Tip:
Golden rule for preparation: Due to the risk of embolization, the surrounding tissue is dissected from the ACC, not vice versa. The vessel should be moved as little as possible.
-
Ligation of the facial vein, partial transection of the digastric muscle
![Ligation of the facial vein, partial transection of the digastric muscle]()
Soundsettings Preparation of the facial vein, which is transected between transfixion ligatures. Transection of the tendinous portions at the anterior edge of the digastric muscle.
Tip:
The facial vein should not be managed with simple ligatures, but always with transfixion ligatures. During emergence from anesthesia or when the patient coughs, high pressures arise in the neck veins, which can lead to simple ligatures slipping off, resulting in intense bleeding.
-
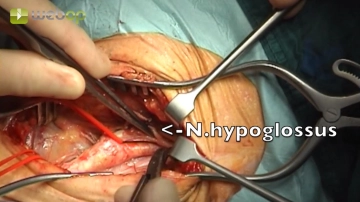
Preparation of the ACE and ACI, Mobilization of the Hypoglossal Nerve
![Preparation of the ACE and ACI, Mobilization of the Hypoglossal Nerve]()
Soundsettings In the cranial wound angle, insertion of a blunt wound retractor and Langenbeck hook. Mobilization of the hypoglossal nerve and the ansa cervicalis. Preparation and retraction of the external carotid artery (ACE). Antefixation of the hypoglossal nerve by a perineural suture to the submandibular musculature. Looping of the internal carotid artery (ACI).
Tips:
1. This surgical step requires the insertion of blunt retractors and hooks in the cranial wound angle. However, no excessive pressure should be applied, as this can otherwise lead to damage to the marginal mandibular branch of the facial nerve (postoperative drooping mouth corner).
2. Preparation only lateral to the ansa cervicalis. If prepared medially, this can impair the vascularization of the hypoglossal nerve.
3. If enlarged lymph nodes are encountered during preparation, they should be medialized en-bloc.
4. Here too: Prepare perivascular tissue away from the vessels, not the other way around.
5. Subtle sparing of the vagus nerve! It usually lies "behind" between the internal carotid artery and the internal jugular vein, but occasionally further "in front" between the vessels. In cases of arteriosclerotically induced perivascular adhesions as in the video example, the extremely sensitive nerve must be carefully detached from the carotid, so that it does not later get caught between the branches of the vascular clamps. The vagus nerve should also not be included in the retractor.
6. If a far peripheral (cranial) exposure of the internal carotid artery is required, one encounters the digastric muscle and occasionally also the glossopharyngeal nerve (N. IX). This nerve must also be carefully spared, as otherwise the patients suffer from extremely distressing coordination disorders when swallowing.
7. Looping of the hypoglossal nerve (N. XII) should be avoided if possible, as this requires unnecessary circular preparation of the nerve. Due to excessive devascularization and moving the nerve back and forth, it can be damaged (consequences: lumpy speech, patient bites ipsilaterally on the tongue while chewing). Instead of looping, temporary suturing of the nerve to the submandibular musculature is possible. For this, only the perineurium is grasped and the suture is placed loosely ("air knot").
-
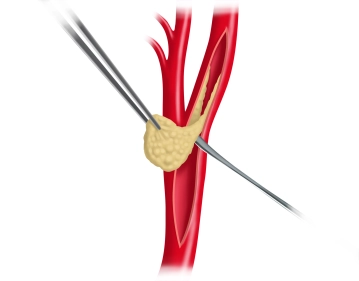
Clamping of the Carotid Bifurcation and TEA
![Clamping of the Carotid Bifurcation and TEA]()
Soundsettings Systemic administration of 5000 IU heparin and waiting for the circulation time. Under pure oxygen ventilation, clamping of the carotid bifurcation: CCA with a 120° clamp, ICA with a soft Gregory clamp, and finally the ECA with a curved clamp. Longitudinal incision of the CCA towards the ICA beyond the peripheral (= cranial) border of the ICA stenosis. Local TEA of the carotid bifurcation using a vascular spatula, which extends peripherally into the ICA without step formation. For preparation of the subsequent shunt insertion, careful dilation of the ICA peripherally using a clamp.
Tips:
1. The superior thyroid artery can, if necessary, be closed with a bulldog clamp.
2. The ICA must be prepared far enough peripherally (= cranially). Otherwise, a dissection can occur, which - if at all - is difficult to control. In case of impending dissection, peripheral intima fixation sutures are disadvantageous, as further dissection or even embolization can still occur.
After secure TEA of the ICA without leaving an intimal step, a shunt tube (usually 5-F) is inserted
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$52.91/ yearly payment
vascular surgery
Unlock all courses in this module.
US$105.80 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.