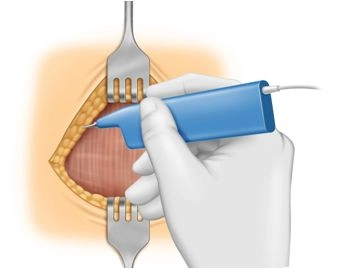
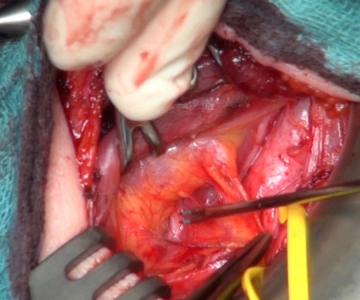
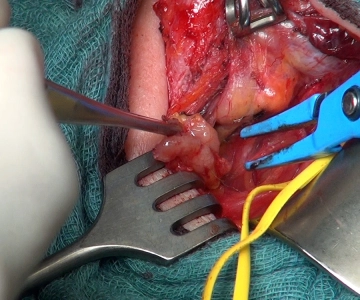
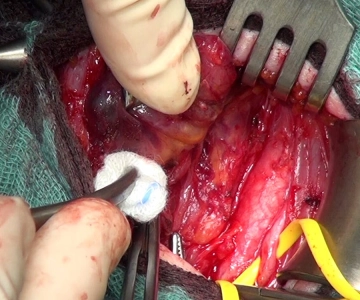
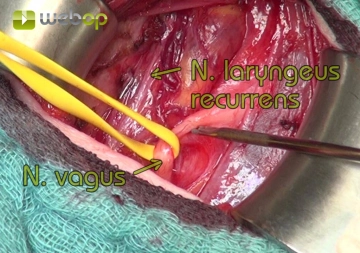
The recurrent laryngeal nerve is visualized on the dorsal side of the left thyroid lobe after careful dissection, confirmed by the use of neuromonitoring.
Note: If the nerve cannot be visualized, the use of neuromonitoring is highly recommended. Initially, the vagus nerve should be stimulated, confirming the regular conduction function of the nerve loop (vagus nerve via the recurrent laryngeal nerve to the vocal muscle). Subsequently, systematic palpation of the retrothyroid space with the stimulation probe until a corresponding acoustic signal is audible and a typical electromyographic curve is visible on the monitor.
Tips for Exposure, Dissection, and Preservation of the Recurrent Laryngeal Nerve
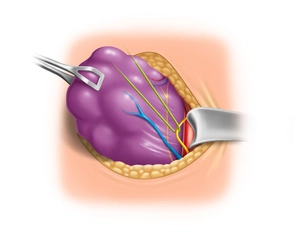
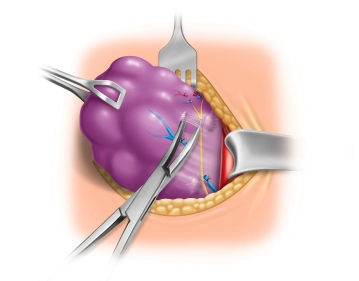
Tip 1: Atraumatic Nerve Exposure
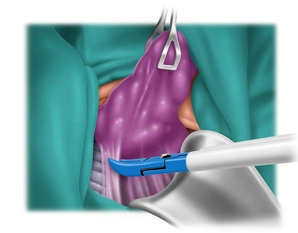
At the suspected location, connective tissue fibers are carefully lifted with atraumatic forceps, and the nerve is exposed with a delicate dissecting clamp, such as a fine Overholt clamp, whose branches are to be guided parallel to it, with spreading movements.
Tip 2: Surgical loupes
The use of surgical loupes is helpful during dissection. The approximately 1 to 2 mm thin nerve is recognizable by its whitish structure with typical vascular markings.
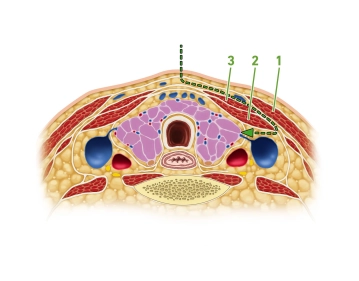
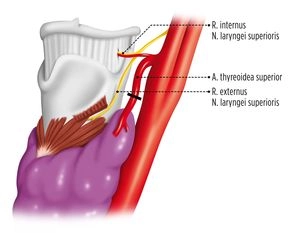
Tip 3: Variability of Nerve Course
If the nerve is not found at its typical location in the esophagotracheal angle, it may be displaced anteriorly from its regular anatomical position by the dislocation of the thyroid, especially if it runs through a vascular bifurcation of the inferior thyroid artery. Special caution is advised in cases of recurrent goiter, and the use of neuromonitoring is therefore highly recommended.
Tip 4: Anatomical Variant
With a frequency of approximately 1%, a non-recurrent laryngeal nerve is found. Here, too, the nerve is not found in its typical location but runs horizontally, or also ascending or descending from the vagus nerve directly to the larynx.