Klatskin tumors are a subgroup of bile duct carcinomas. The term Klatskin tumor encompasses the entity of perihilar bile duct tumors between the junction of the cystic duct and the branches up to the second generation of the right and left bile duct.
Etiology
The current concept for the development of bile duct carcinomas is based, similar to gastrointestinal tract carcinomas, on the so-called adenoma-carcinoma sequence. This is thought to be triggered by a combination of chronic inflammatory changes with increased cell turnover and prolonged or recurrent cholestasis. Predisposing conditions are therefore congenital abnormalities of the bile ducts such as Caroli syndrome, choledochal cysts, abnormal junction of the bile ducts, and inflammatory stenosing bile duct diseases such as sclerosing cholangitis or liver fluke infection.
Bismuth-Corlette Classification
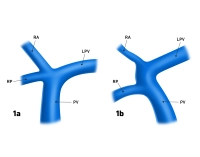
Hilar cholangiocarcinomas were first described by Klatskin in 1965. Ten years later, Bismuth et al. classified the ECC (extrahepatic cholangiocarcinomas) according to their anatomical pattern of involvement. This clinical-surgical classification is based solely on the spread of the carcinoma along the bile ducts and distinguishes four main types:
I. The carcinoma affects only the main bile duct distal to the bifurcation.
II. The tumor is located in the area of the bifurcation without involvement of the right and left bile ducts.
III. Both the bifurcation and the right or left bile duct are affected, with IIIa indicating involvement of the right and IIIb indicating involvement of the left bile duct.
IV. Extensive tumor growth along the bile ducts with involvement of the bifurcation and both bile ducts, including second-order branches or discontinuous tumor growth.
Regional Lymph Nodes
The regional lymph nodes of perihilar bile duct carcinoma are only the hilar and pericholedochal lymph nodes in the hepatoduodenal ligament.