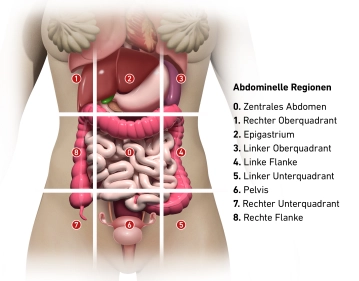
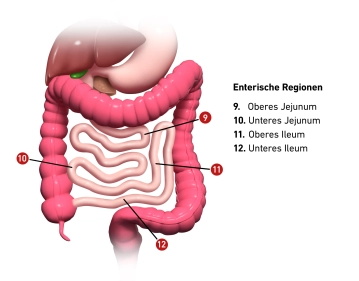
The Sugarbaker Index, also known as the Peritoneal Cancer Index (PCI), is a scoring system used to determine the tumor burden and distribution in peritoneal carcinomatosis. The PCI divides the abdominal cavity into 13 regions, of which 9 are abdominal and 4 are enteric areas.
Abdominal regions
0. Central abdomen
1. Right upper quadrant
2. Epigastrium
3. Left upper quadrant
4. Left flank
5. Left lower quadrant
6. Pelvis
7. Right lower quadrant
8. Right flank
Enteric regions:
9. Upper jejunum
10. Lower jejunum
11. Upper ileum
12. Lower ileum
In each of these 13 regions, the size of the largest tumor deposit is assessed and scored as follows:
- 0 = No visible tumor deposits
- 1 = Tumor deposits up to 0.5 cm
- 2 = Tumor deposits 0.5 - 5 cm
- 3 = Tumor deposits > 5 cm or confluence
The scores of all 13 regions are then summed to a total score (PCI 0-39), reflecting the extent of peritoneal carcinomatosis.
| Region | Organs to be assessed |
|---|---|
| 0 - Central | Midline abdominal incision – Greater omentum – Transverse colon |
| 1 - Right upper | Surfaces of the right liver lobe – Underside of the right diaphragm – Right retrohepatic space |
| 2 - Epigastrium | Epigastric fat pad – Left liver lobe – Lesser omentum – Falciform ligament |
| 3 - Left upper | Underside of the left diaphragm – Spleen – Tail of the pancreas – Anterior and posterior surfaces of the stomach |
| 4 - Left flank | Descending colon – Left paracolic gutter |
| 5 - Left lower | Pelvic wall lateral to the sigmoid colon – Sigmoid colon |
| 6 - Pelvis | Female internal genitalia with ovaries, fallopian tubes, and uterus – Bladder, Douglas pouch – Rectosigmoid |
| 7 - Right lower | Right pelvic wall – Appendix |
| 8 - Right flank | Right paracolic gutter – Ascending colon |
| 9 - Upper jejunum | |
| 10 - Lower jejunum | |
| 11 - Upper ileum | |
| 12 - Lower ileum |