Esophagus
General Characteristics
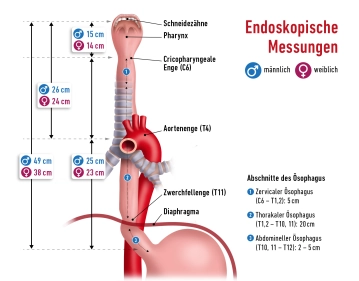
- Muscular hollow organ, approx. 25–30 cm long
- Connects pharynx (C6) with the stomach (Th11)
- Three constrictions:
- Upper constriction – cricoid constriction (transition pharynx/esophagus, at level C6)
- Middle constriction – aortic constriction (crossing with aortic arch + left main bronchus)
- Lower constriction – diaphragmatic constriction (esophageal hiatus, Th10)
Topographical Sections
Cervical Esophagus (C6–Th1)
- Behind the trachea
- Accompanying structure: recurrent laryngeal nerve
- Access: transcervical, ventral-lateral
Thoracic Esophagus (Th1–Th10)
- Upper mediastinum: behind trachea, in front of spine
- Middle mediastinum: behind heart and pericardium
- Crossing by aortic arch, azygos vein, left main bronchus
- Access: right-thoracic (better overview)
Abdominal Esophagus (short, 1-3 cm)
- Passes through esophageal hiatus (Th10) into the abdomen
- Empties into the cardia region of the stomach
- Accompanying structures: anterior vagal trunk (left), posterior (right)
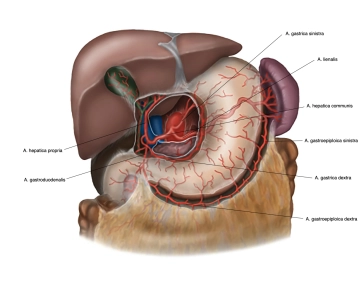
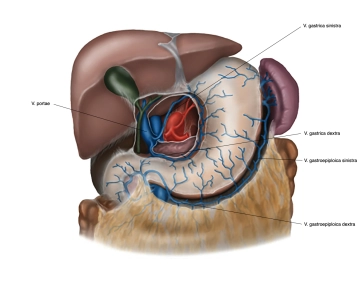
Stomach
General & Location
- Muscular hollow organ between esophagus and duodenum
- Located in the left/middle upper abdomen, directly under the diaphragm
- Can vary greatly in size and shape depending on age, filling state, and body position
- Great interindividual differences in terms of location, size, and shape
Size & Filling Capacity
- Average length: 25–30 cm (with moderate filling)
- Storage capacity: approx. 1.5 liters, in extreme cases up to 2.5 liters
Stomach Layers and Attachment
- Located intraperitoneally; mostly covered with serosa (except dorsal cardia)
- Embryonic mesogastria rotate into a frontal position:
- Lesser omentum: from the lesser curvature to the hepatic portal
- Greater omentum: from the greater curvature to the transverse colon, spleen, and diaphragm
- Attachment and stabilization by ligaments that, among other things, extend to the liver and spleen
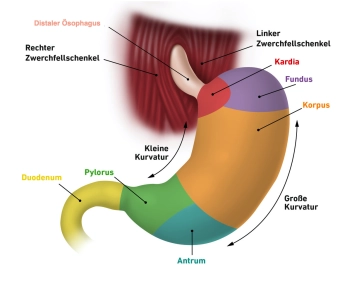
Sections of the Stomach
- Cardia (stomach entrance, upper gastric orifice, ostium cardiacum)
- Area of 1–2 cm in which the esophagus empties into the stomach
- Distinct transition from esophageal mucosa to gastric mucosa (clearly visible on endoscopy)
- Gastric Fundus (stomach fundus)
- Located above the stomach entrance, bulges upward
- Also referred to as gastric dome or fornix gastricus
- Typically filled with air; in upright position the highest point, recognizable as “gastric bubble” on X-ray
- Delimited from the stomach entrance by the cardiac notch
- Gastric Corpus (stomach body)
- Main part of the stomach
- Characterized by deep longitudinal mucosal folds (plicae gastricae) that run from the stomach entrance to the pylorus (“gastric canal”)
- Pylorus (pyloric part, pyloric sphincter)
- Beginning with the expanded pyloric antrum, followed by pyloric canal (canalis pyloricus)
- Ends with the actual pyloric sphincter (pylorus), where the pyloric sphincter muscle (M. sphincter pylori) is located
- Closes the stomach outlet (ostium pyloricum) and regulates the passage of chyme into the duodenum
Formal Boundaries and Further Anatomical Features
- Greater curvature (convex side)
- Lesser curvature (concave side)
- Anterior wall: Paries anterior; Posterior wall: Paries posterior
- Greater omentum originates from the greater curvature; Lesser omentum spans between the left hepatic lobe and the lesser curvature