The TASC II criteria recommend therapeutic treatment options depending on the length of the local occlusion/stenosis. The length of the stenosis and its regional location determine the treatment: endovascular or open vascular surgery.
TASC II classification of aortoiliac lesions
Type | Morphology | Procedure |
A | Unilateral or bilateral CIA stenosis; unilateral or bilateral short single (<3 cm) EIA stenosis | Endovascular |
B | Single or multiple stenosis totaling 3–10 cm involving the EIAnot extending into the CFA and/or unilateral CIA occlusion | Endovascular |
C | Bilateral CIA stenoses; bilateral EIA stenosis, 3–10 cm long, not extending into the CFA; unilateral EIA occlusion; bilaterasl CIA occlusions | Open revascularization |
D | Diffuse disease involving the aorta and both iliac arteries requiring treatment; bilateral EIA occlusions; unilateral occlusions of both CIA and EIA; infrarenal aortoiliac occlusion; diffuse multiple stenosis involving the unilateral CIA, EIA and CFA | Open revascularization |
Video example:
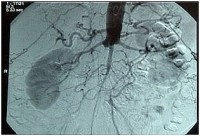
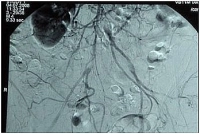
High aortic occlusion with subtotal stenosis of the iliac bifurcation, occlusion of the right CIA and thrombosis at the left EIA (bilateral clinical Fontaine stage IIb).
-> TASC II D, hence recommendation for open revascularization
Preoperative intra-arterial DSA
Classification of PAD according to Fontaine stage and Rutherford category
Fontaine stage | Presentation | Rutherford category | Grade | Presentation |
I | Asymptomatic | 0 | 0 | Asymptomatic |
IIa | Mild claudication (> 200 m) | 1 | I | Mild claudication |
IIb | Moderate to severe claudication (< 200 m) | 2 | I | Moderate claudication |
| 3 | I | Severe claudication | |
III | Ischemic rest pain | 4 | II | Ischemic rest pain |
IV | Ulceration or gangrene | 5 | III | Minor tissue loss |
6 | III | Major tissue loss |