Approximately 80% of abdominal aortic aneurysms are located infrarenally. However, in up to 20%, there is no sufficient aneurysm neck (juxtarenal aneurysm), and the AAA can also begin at or above the renal arteries (suprarenal aneurysm). The missing or morphologically inadequate infrarenal anchoring zone („hostile neck“) excludes a conventional endovascular aneurysm exclusion.
Fenestrated prostheses or the chimney technique (Ch-EVAR = „chimney technique with endovascular aneurysm repair“) allow these pathologies to be treated endovascularly. The chimney technique creates a proximalization of the landing zone to ensure the necessary anchoring for the abdominal stent graft. This is achieved by implanting a usually covered stent (chimney graft) into the affected renovisceral vessel of the aorta, parallel and outside the aortic endoprosthesis.
The indications for the treatment of pararenal pathologies using the chimney technique include:
- large rupture-prone aneurysms (> 6 cm diameter) or penetrating aortic ulcers without thrombus formation
- abdominal aneurysms with „hostile neck“ and pronounced angulation/calcification of the iliac arteries and/or the aneurysm neck
- symptomatic, ruptured pathologies
- Type Ia endoleak after previous EVAR
- Presence of relevant, accessory or ectopic renal arteries with a diameter of more than 4 mm
- paraanastomotic aneurysms after previous open aneurysm treatment
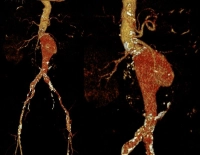
In the video example, it is a symptomatic abdominal aortic aneurysm with 9.5 cm diameter at the level of the renal arteries (juxtarenal), accompanying CAD, s/p pacemaker implantation right prepectoral:
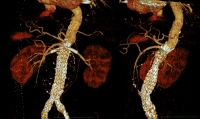
Postoperative: