- Abdominal aortic aneurysm (AAA) > 5 cm
- smaller aneurysms in eccentric AAA or ulcerations with contained perforation (PAU, penetrating aortic ulcer)
- symptomatic aneurysms of any size
Special indications and therapy options for Behçet's disease, Marfan syndrome, mycotic aneurysms such as e.g. Salmonella infections and AAA with peripheral embolization.
The indication for invasive therapy of an abdominal aortic aneurysm (AAA) basically results from a comparison of the individual rupture risk in the natural course against the surgical risk. If the rupture risk in the natural course exceeds the individual surgical risk, the indication for invasive therapy is generally given.
Classification of Rupture Risk
Factors | Low Risk | Medium Risk | High Risk |
|---|---|---|---|
Aneurysm diameter | < 5 cm | 5-6 cm | > 6 cm |
Growth rate per year | < 0,3 cm | 0,3-0,5 cm | > 0,5 cm |
Smoking/COPD | low | moderate | high |
Family history | none | isolated | frequent |
Arterial hypertension | none | well controlled | unstable despite therapy |
Morphology | fusiform | saccular | bulges |
Gender | male | female |
Surgical Indication
Classification | Size | Wall | Clinical presentation | Surgical Indication |
|---|---|---|---|---|
asymptomatic infrarenal | > 5 cm ♂ > 4,5 cm ♀ | intact | none | elective |
asymptomatic suprarenal | > 6 cm | intact | none | elective |
symptomatic | independent | intact | Spontaneous pain, tender abdomen, back or flank | urgent, within 24 hrs. |
ruptured | independent | contained or free ruptured | diffuse severe spontaneous/touch pain of the tense abdomen, with/without hemorrhagic shock | Emergency |
aortoduodenal fistula | intermittent vomiting, melena | Emergency | ||
aortocaval fistula | Right heart failure, fistula sounds, truncal cyanosis, simultaneous contrast enhancement aorta & inferior vena cava | Emergency |
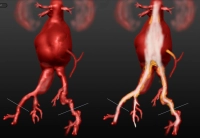
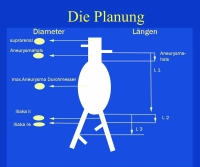
For the surgical treatment of the AAA, two procedures are available:
- the open replacement of the abdominal aorta with a tube or bifurcation prosthesis (OAR, open aortic repair)
- the endovascular implantation of a stent prosthesis (EVAR, endovascular aortic repair)
Laparoscopic aneurysm surgery, usually in combination with a mini-laparotomy, is of rather minor importance.
For the selection of the procedure - OAR or EVAR - the following recommendations exist:
OAR (trans-, retroperitoneal)
- normal life expectancy
- low surgical risk ( “fitness”)
- unsuitable anatomy for EVAR: landing zone, aneurysm neck (angle, length), iliac vessels (stenoses, elongation, kinking), thrombi, calcification
- Marfan and other connective tissue diseases
EVAR (standard prosthesis, custom-made)
- previous abdominal operations
- limited life expectancy
- high surgical risk
- anatomy suitable for EVAR (see above)
EVAR requires adequate iliac vessels for access, as the stent graft systems are often large-caliber. Problematic are atherosclerotically narrowed, tortuous and kinked, but also aneurysmatically dilated iliac vessels.
In the long-term course, the endovascular aortic prosthesis is associated with a higher complication rate than open aortic surgery.
The mortality risk for EVAR or OAR of an individual patient can be quickly calculated using the so-called BAR Score Calculator → www.britishaneurysmrepairscore.com, which can be usefully used for patient counseling about the risk of an elective procedure with EVAR or OAR.
The general surgical indication is given for (isolated) iliac aneurysm from an aneurysm diameter of 3 cm.
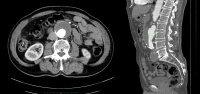
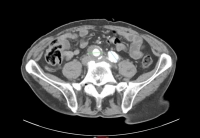
Video example:
- infrarenal AAA, diameter 54.2 mm
- aneurysm of the right common iliac artery, diameter 41.1 mm