Stenosis or occlusion of the subclavian artery with clearly attributable symptoms:
- clinically relevant vertebrobasilar insufficiency that is reproducible by provocation tests
- hypoperfusion of the arm requiring treatment (brachial claudication)
Start your free 3-day trial — no credit card required, full access included
Stenosis or occlusion of the subclavian artery with clearly attributable symptoms:
History
Clinical-Neurological Examination
1. Cerebral Symptoms
2. Peripheral Symptoms
Doppler and Duplex Sonography
In the ultrasound examination of the extracranial brain-supplying vessels, all vessels should always be assessed in transverse and longitudinal sections:
Both the brachiocephalic trunk and the origin area of the left subclavian artery are usually not directly visible for anatomical reasons. However, from the flow spectrum of the more cranial arterial sections, stenoses in the inflow can be indirectly inferred (fist closure test, application of a blood pressure cuff → flow reversal).
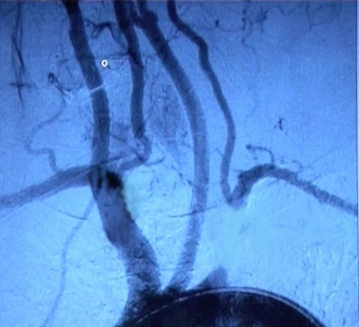
Digital Subtraction Angiography (DSA), MR Angiography
CT or MRI Brain
Cardiological Examination
Chest X-ray Examination
Laboratory
General Surgical Risks
Specific Surgical Risks
Activation of this course for 3 days.
Most popular offer
Combine our learning modules flexibly and save up to 50%.
US$52.30/ yearly payment
Unlock all courses in this module.
US$104.60 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.