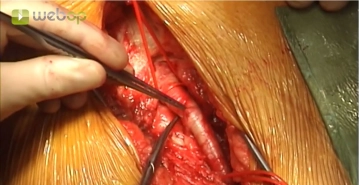
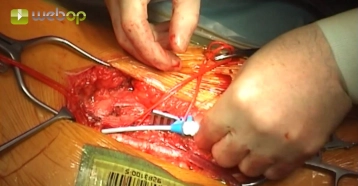
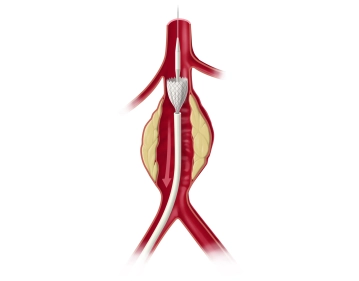
Approximately 1 cm lateral to the palpated femoral artery make a longitudinal skin incision on the proximal thigh distal to the inguinal aspect. After transecting the subcutaneous tissue, divide the femoral fascia longitudinally medial to the sartorius muscle. Open the fascia of the adductor canal at the distal edge of the incision, expose the superficial femoral artery, and encircle it with a vessel loop. Divide and suture ligate between Overholt forceps the lymph collectors crossing posterior to the inguinal ligament. Encircle the common and deep femoral arteries with vessel loops.
Repeat these steps to expose the femoral bifurcation in the left groin.
Tips:
1. Access lateral to the femoral artery spares the lymph collectors and permits subsequent offset layered closure to promote effective wound healing.
2. The superficial femoral artery serves as a landmark for proximad dissection lateral to it. This helps to easily locate the deep and common femoral arteries and also avoids the risk of injury to the veins running medially.
3. Suture ligation of the lymph collectors helps, to a large extent, to prevent subsequent lymphatic cysts and fistulae. Postoperative lymph collection in the groin often paves the way for deep wound infection with fatal consequences.
4. Lateral and medial circumflex femoral arteries: at times, these arteries are hidden and can bleed profusely if not clamped.